Preeclampsia (also called toxemia) is a condition seen with high blood pressure at or after 20 weeks of pregnancy in a woman whose blood pressure was normal before pregnancy.
Additional to high blood pressure, increased swelling of the body parts, and protein in the urine are other findings of preeclampsia. If it is severe enough to affect brain function, it leads to seizures or coma, turning to eclampsia.
Preeclampsia is seen in 5-8% of pregnancy. It can be managed without any serious risk by catching it at the early stages. It can be detected early by routine blood pressure measurements and urine tests with each prenatal visit.
Watch: Pregnancy Complications - PreeclampsiaHigher Risk Groups for Preeclampsia:
Preeclampsia is seen more often with first pregnancies, and those mothers have higher risks of preeclampsia in their future pregnancies. Other risk factors are:
- Hypertension before pregnancy
- Kidney disease before pregnancy
- Diabetes before pregnancy
- Obesity
- Older age
- Multiple gestations
- Family history of preeclampsia, genetic predisposition
- Rheumatoid arthritis, lupus, scleroderma, multiple sclerosis, and sickle cell disease also bring increased risks for preeclampsia
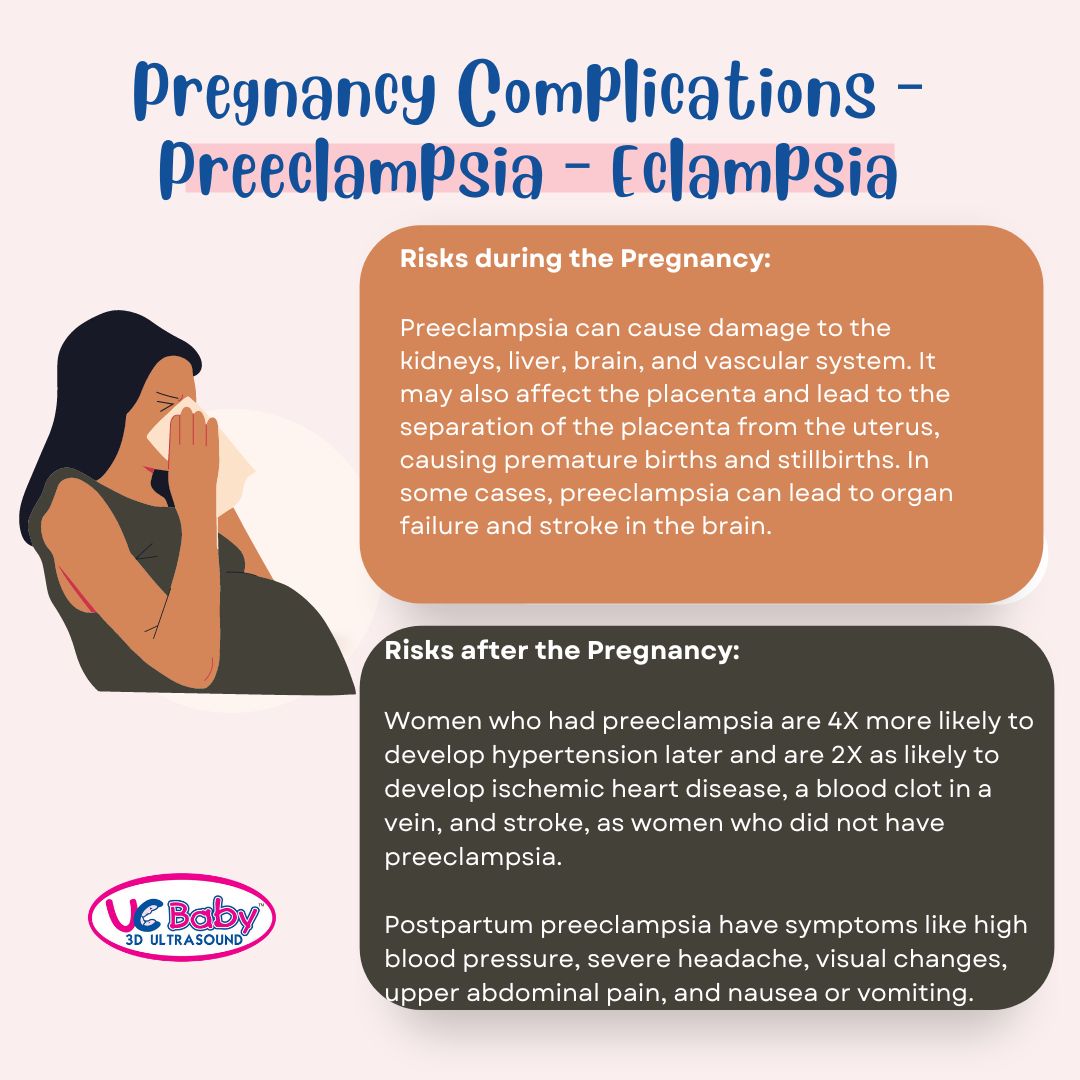
Risks during the Pregnancy:
Preeclampsia can cause damage to the kidneys, liver, brain, and vascular system. It may also affect the placenta and lead to the separation of the placenta from the uterus, causing premature births and stillbirths. In some cases, preeclampsia can lead to organ failure and stroke in the brain.
When preeclampsia goes to the eclampsia stage, causing seizures, the woman loses consciousness and twitches uncontrollably. If the fetus is not delivered at that stage, these conditions can cause the death of the mother and/or the fetus.
According to the WHO, preeclampsia and eclampsia cause 14% of maternal deaths each year, or about 50,000 to 75,000 women worldwide.
Risks after the Pregnancy:
In “uncomplicated preeclampsia,” the mother’s high blood pressure and other symptoms usually go back to normal within six weeks of delivering the baby. However, women who had preeclampsia are four times more likely to develop hypertension later and are twice as likely to develop ischemic heart disease, a blood clot in a vein, and stroke as women who did not have preeclampsia.
Less commonly, mothers who had preeclampsia can experience permanent damage to their kidneys and liver. They can also experience fluid in the lungs. In addition, in the days following birth, women with preeclampsia remain at increased risk for developing eclampsia and seizures.
In some cases, preeclampsia develops between 48 hours and six weeks after they deliver their baby—a condition called postpartum preeclampsia. The symptoms include high blood pressure, severe headache, visual changes, upper abdominal pain, and nausea or vomiting.
It is essential to recognize and treat postpartum preeclampsia and eclampsia because the risk of complications is higher than if the condition had occurred during pregnancy.
Postpartum preeclampsia and eclampsia can progress very quickly if not treated and may lead to stroke or death. Therefore, moms need to continue to monitor their health after delivery as any mother can have postpartum preeclampsia after delivering a baby.
Can Preeclampsia & Eclampsia be prevented?
There is no way known to prevent preeclampsia and eclampsia. However, the outcome can be improved with prompt recognition and management, so pregnant women need to have routine health screenings. If you are at high risk, the doctor may recommend taking a low dose of aspirin starting after 12 weeks of pregnancy to help prevent preeclampsia.
Risks of Preeclampsia & Eclampsia to the Baby:
Preeclampsia may be related to problems with the placenta early in the pregnancy and issues that pose risks to the fetus, including:
- Impaired fetal growth with decreased oxygen and nutrients supply
- Preterm birth
- Stillbirth if placental abruption leads to heavy bleeding in the mother
- Infant death
- Increased risk for problems later (including learning disorders, cerebral palsy, epilepsy, deafness, and blindness)
- Poor growth in the uterus may later be at higher risk of diabetes, congestive heart failure, and high blood pressure.
Treatment for Preeclampsia & Eclampsia:
Treatment protocols depend on how severe the condition is, the potential for maternal complications, how far along the pregnancy is, and the potential risks to the mother and fetus. The risks can be kept minimized by continuous medical care to the mother while giving the fetus as much time as possible for maturation before delivery.
Note: The information on this blog is not meant to diagnose or be intend to provide full coverage on the topic of preeclmpaisa of eclampsia. For more information and clarification, contact your health care practitioner.
REFERENCES:
About Preeclampsia and Eclampsia
Postpartum Preeclampsia: Moms are still at Risk after Delivery
Pregnancy: Preeclampsia vs.Eclampsia
Preventing Preeclampsia: Questions for the Doctor
Written by: Tina I Ureten MD, RDMS, RDCS
Read our blog on – Stages and Phases of Childbirth





 Invite families and friends to witness this memorable event of your pregnancy. Celebrate that special child-bonding moment with your loved ones, wherever they are in the world.
Invite families and friends to witness this memorable event of your pregnancy. Celebrate that special child-bonding moment with your loved ones, wherever they are in the world. There is nothing more beautiful than your baby's heartbeats. Save that sound forever in a UC Baby® Heartbeat Bear®. It's not just a great keepsake, but also an effective way to sooth your baby to sleep.
There is nothing more beautiful than your baby's heartbeats. Save that sound forever in a UC Baby® Heartbeat Bear®. It's not just a great keepsake, but also an effective way to sooth your baby to sleep.

